5 Common Paperwork Mistakes That Compromise Patient Safety
Paperwork Errors That Put Patients at Risk
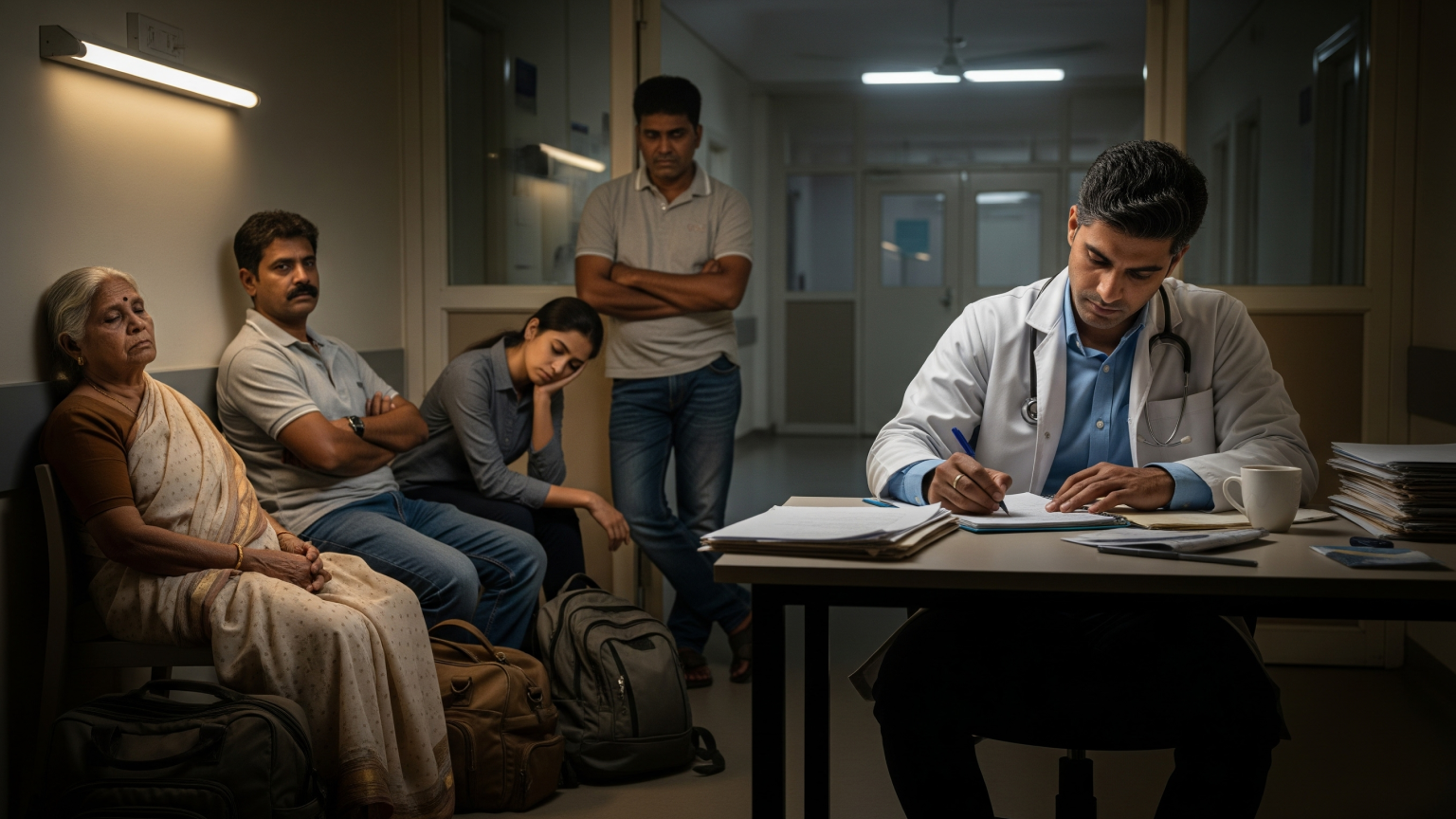
In hospitals, patient safety is usually linked to clinical care — correct diagnoses, safe surgeries, or timely medications. But behind every treatment is another critical factor: paperwork.
Discharge summaries, progress notes, prescriptions, and insurance documents all shape the patient’s journey. When paperwork is inaccurate, delayed, or incomplete, it can create serious risks. Families may leave without proper instructions, claims may get rejected, and in some cases, medical errors can occur.
Unfortunately, paperwork mistakes are more common than many hospitals realize. Here are five of the most frequent errors — and how they compromise patient safety.

One of the most common issues is missing or incomplete discharge documentation. Patients may leave the hospital without:
This can lead to confusion at home, missed treatments, and avoidable readmissions. For hospitals, it also means blocked beds and dissatisfied patients.
Handwritten notes are still common in many hospitals, but they pose major risks. Doctors and nurses often struggle to interpret unclear handwriting or shorthand.
For example, a dosage written incorrectly can cause serious harm. Similarly, when notes aren’t structured in NABH/JCI-compliant formats, staff waste hours trying to reorganize data. These delays affect both clinical accuracy and operational efficiency.

NABH and JCI standards require structured documentation with specific fields. When these fields are left blank or filled inconsistently, hospitals face:
What looks like a small paperwork gap can snowball into financial loss and reputational damage.
Paperwork often lags behind patient care. Doctors may discharge patients first and complete summaries later, or MRD staff may wait hours for handwritten notes to be corrected.
The consequences include:
Every hour of delay adds stress for families and lost efficiency for the hospital.

Incorrect use of ICD codes or medical terminology is another frequent issue. Mistakes here can:
For patients, this may result in missed treatments or financial disputes. For hospitals, it creates avoidable revenue leakage.

While paperwork errors seem inevitable in busy hospitals, they don’t have to be. AI-powered tools like Patient Lens AI help prevent these mistakes by embedding accuracy and compliance into daily workflows.
Key features include:
Because the system combines AI drafting with human verification, it balances speed with trust — ensuring safe, compliant, and patient-friendly documentation.

Fixing paperwork mistakes isn’t just about avoiding audits or reducing denials. It’s about patient safety. With accurate, complete, and timely documentation, hospitals can:
One hospital administrator summed it up well: “Earlier, discharge paperwork was our biggest source of complaints. Since adopting AI, patients leave on time with complete instructions, and our audits are smoother than ever.”
👉 Book a demo today to see how Patient Lens AI prevents paperwork mistakes and makes every discharge safer and faster.
A writer exploring the intersection of healthcare, technology, and patient care, bringing clarity to complex topics through engaging storytelling.